The MP-eye uses a persons' ability to see the shadow created on their retina by their own macular pigments in polarized light (known as Haidinger's brushes) to determine the amount of macular pigment present. This new approach is fast enough to fit into a regular eye exam and easy enough that everyone from 5-95 years old can have their macular pigments assessed.
The MP-eye assesses how much macular pigment is in the eye. Macular pigments only come from your diet and low levels have been linked to an increased risk of blindness.

What does the MP-eye do?
Macular Pigment Assessment
Macular pigments in the eye protect the retina from short-wavelength, high-energy (violet-blue, 380-500 nm) light and the damaging effects of oxidization by free radicals (reactive oxygen species). They do this by absorbing as much as 90% of the harmful blue light and acting as antioxidants (for review, see [1]). The higher the density of macular pigments, the greater the protection for the retina. The MP-eye assesses the amount of macular pigment present, thereby providing a measure of the eye's natural defences against blue light and free radicals.
How the MP-eye works
A Psychophysical Threshold Test
The MP-eye produces a visual effect in the eye that becomes increasingly difficult to see. The test works by measuring the patient's threshold for seeing this effect, like how a Snellen or LogMAR chart is used to estimate visual activity. For the MP-eye, the greater the amount of macular pigment the easier the effect is to see. And as the MP-eye makes the task harder, the more steps a patient with high macular pigments will be able to see therefore scoring a lower threshold (higher MP-eye score), which is better. The patient is actively involved in the process as they must observe the effect and report if they can see it, or not, just like a visual fields test.
Haidinger's Brushes
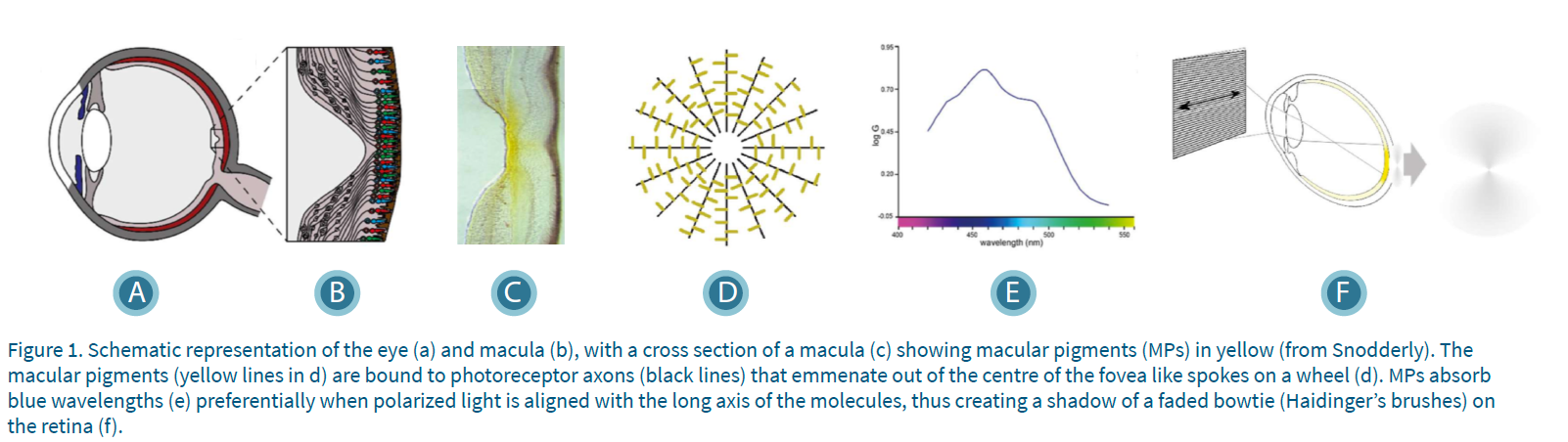
The MP-eye uses a visual effect known as Haidinger's brushes, which is caused by the way macular pigments absorb polarized light. Macular pigments are long thin molecules that preferentially absorb violet-blue light when the plane of polarization of the light is aligned with the long axis of the macular pigment molecule [2].
The macular pigments are attached in a perpendicular orientation to the photoreceptor axons [3] that form the Henle nerve fiber layer, which emanates out of the center of the fovea like the spokes of a wheel [4]. This alignment creates a pattern of concentric circles of macular pigment centred on the fovea.
When linearly polarized white light is observed by the retina, the absorption of the violet-blue light by the macular pigments creates a yellow shadow on the retina, where the macular pigments are aligned with the angle of the incoming polarized light. The pattern of this subtle yellow shadow has been described as a bow-tie, hourglass or propeller and is known as Haidinger's brushes [5].
How well a person can perceive Haidinger's brushes is a function of the density of their macular pigments, which is the underlying principle used by the MP-eye [6-8].
Optimizing the Effect
The Haidinger's Brushes effect is subtle, so the MP-eye uses a special lighting environment to optimize conditions for seeing the effect. Haidinger's brushes would normally disappear within 2-5 seconds as the brain quickly adapts to static images (Troxler effect), so the MP-eye uses a rotating polarizer to maintain the effect indefinitely.
The patient will see the Haidinger's brushes rotating clockwise or anti-clockwise depending on the rotation direction of the polariser and they are asked to report the direction of rotation that they observe.
Reaching Threshold
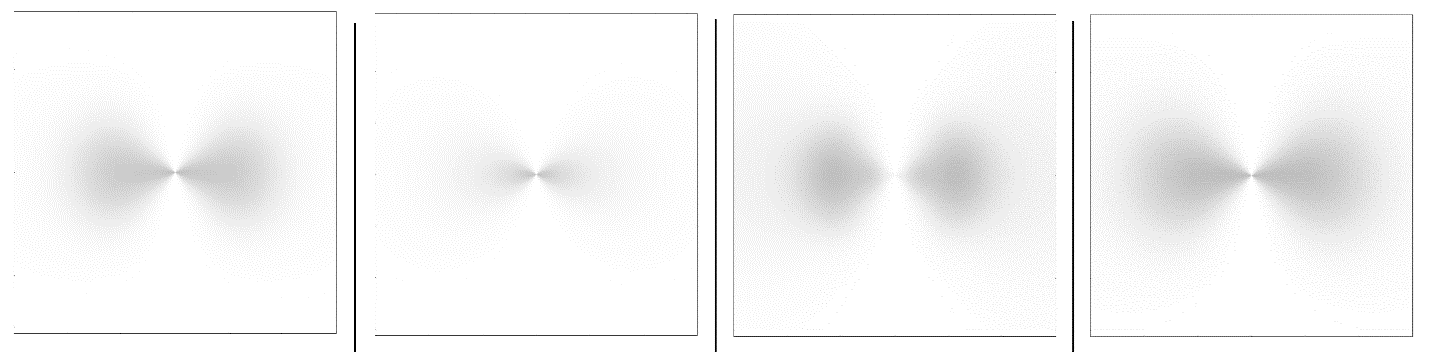
The MP-eye uses patented filters that decrease the amount of light that is polarized (degree of polarization), making the Haidinger's brushes effect increasingly difficult to see [6,7].
Threshold Indicates Macular Pigment Volume
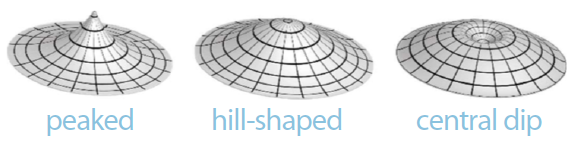
Due to the different patterns of macular pigment density that people have (peaked, central dip, etc.)[9-11] it is more useful to measure the total volume of macular pigment than just a single eccentricity.
Clinical research has shown that a person's ability to perceive Haidinger's brushes using the MP-eye is related to the total volume of macular pigments in the macula [7]. People who see Haidinger's brushes at a low degree of polarization have higher levels of macular pigmentation. The MP-eye decreases the degree of polarization in 10 steps and therefore provides a score out of 10.
Why use the MP-eye?
Know the Score
For the first time, the MP-eye enables eye care professionals to assess their patients' total macular pigmentation (macular pigment volume) as part of a regular eye exam. Every individuals' macular pigment levels are unique to them and this not only determines how much natural protection they have against long-term light damage, but it also affects aspects of their vision such as contrast sensitivity and glare.
Knowing a patient's score means eye care professionals can better tailor their advice and products to that individual to support them in maintaining their long-term eye health.
Empower Patients to Take Action
Patients with low natural defences can be advised to take actions that will help protect their eyes.
Who to test with the MP-eye
Anyone with normal vision can be tested with the MP-eye and they only need to be able to indicate the direction of rotation (clockwise or anti-clockwise) verbally or with some other form of communication, such as hand movements.
Patients with the following conditions may not be able to see the Haidinger's brushes:
- Colour Blindness
- Excessive damage of papillomacular bundle
- Acuity less than 6/60
- Corneal opacities that reduce visual acuity below 6/30
- Vitreous opacities due to uveitis with VA less than 6/22
- Widespread damage to the macula
- Absence of macular pigment
- Macular lesions
- Diabetic maculopathy
- Traumatic edema of the macula
- Macular deterioration due to keratitis and uveitis
- Amblyopia
- Eccentric Fixation
Interested in learning more? Check out some of our related topics
References
- Arunkumar, R., et al., What do we know about the macular pigment in AMD: the past, the present, and the future. Eye, 2018. 32(5): p. 992- 1004.
- Bone, R.A. and J.T. Landrum, Macular pigment in Henle fiber membranes: a model for Haidinger's brushes. Vision Research, 1984. 24(2): p. 103- 108.
- Bhosale, P. and P.S. Bernstein, Vertebrate and invertebrate carotenoid-binding proteins. Archives of Biochemistry and Biophysics, 2007. 458(2): p. 121-127.
- Trieschmann, M., et al., Macular pigment in the human retina: histological evaluation of localization and distribution. Eye, 2008. 22(1): p. 132-137.
- Haidinger, W.K., Über das direkte Erkennen des polarisierten Lichts und der Lage der Polarisationsebene. Annalen der Physik, 1844. 139(9): p. 29-39.
- Temple, S.E., et al., Perceiving polarization with the naked eye: characterization of human polarization sensitivity. Proceedings of the Royal Society Biological Sciences Series B, 2015. 282(1811): p. 20150338.
- Temple, S.E., N.W. Roberts, and G.P. Misson, Haidinger’s brushes elicited at varying degrees of polarization rapidly and easily assesses total macular pigmentation Journal of the Optical Society of America A, Optics and Image Science, 2019. 36(4): p. B123-B131.
- Muller, P.L., et al., Perception of Haidinger brushes in macular disease depends on macular pigment density and visual acuity. Investigative Ophthalmology & Visual Science, 2016. 57(3): p. 1448-1456.
- Robson, A.G., et al., Macular pigment density and distribution: comparison of fundus autofluorescence with minimum motion photometry. Vision Research, 2003. 43(16): p. 1765-1775.
- Green-Gomez, M., et al., Standardizing the Assessment of Macular Pigment Using a Dual- Wavelength Autofluorescence Technique. Translational Vision Science & Technology, 2019. 8(6): p. 13.
- Sharifzadeh, M., P.S. Bernstein, and W. Gellermann, Nonmydriatic fluorescence-based quantitative imaging of human macular pigment distributions. Journal of the Optical Society of America A, Optics, Image Science, and Vision, 2006. 23(10): p. 2373-2387.
