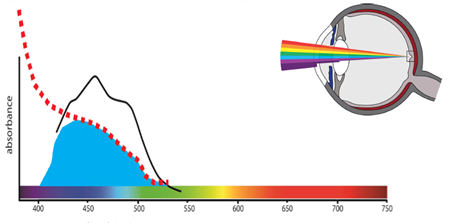
The blue/violet end of the visible spectrum is known as high-energy visible (HEV) light. Like UV radiation, HEV carries enough energy per photon to cause photochemical damage to living cells over time specifically light in the 380-455 nm range.
The cornea and lens block most UV radiation but HEV light penetrates through to the retina where it causes both thermal (type 1) and photochemical (type 2) damage.
While retinal cells do have repair mechanisms, they do not regenerate like other cells in the body (e.g. skin cells that are also exposed to HEV are replaced every 5 days). Through life exposure to HEV light leads to accumulation of irreparable damage to DNA leading to retinal cell death.
The most intense source of blue light is the sun and reflections thereof, but industrial and home lighting are getting dangerously bright and the long time periods that we use digital devices may make them a threat to accumulation of damage. And we increase our risk when they are used in the dark as our pupils dilate letting in as much as 10 times more light, so we should be cautious about long-term use of digital devices.
How Does Blue Light Effect our Eyes?
Blue light can ionize a molecule so that it loses an electron. This turns molecules like lipofuscin into a free radical/reactive oxygen species, which can interact with other cellular components to cause short term (repairable) and long-term (irreparable damage, i.e. to DNA or mitochondrial DNA).
The accumulation of blue light damage to photoreceptor outer segments or to the recycling mechanism of the retinal pigmented epithelium (RPE) cells, can cause a build-up of waste products called drusen that separate the photoreceptors of the macula from their sole blood supply from the choroid, leading to cell death and geographic atrophy.
Drusen is the hallmark of the onset of age-related macular degeneration.
.jpg?width=268&height=178&name=sebastian-coman-travel-dtOTQYmTEs0-unsplash%20(1).jpg)

Because blue light photochemical damage is all about exposure, which is intensity x time, if we can reduce the intensity by using hats, sunglasses, blue light filtering lenses, or increasing our bodies natural defence by taking supplements then we can reduce the rate of accumulation of damage. If we can slow the rate of damage then AMD may not develop during a person’s living years, so thereby preventing the disease.
Science Behind the Danger of Blue Light to the Retina
There is a wealth of evidence that the blue end of the visible spectrum of light is most dangerous to the retina. Ultraviolet and infrared are almost entirely filtered out by the lens, cornea and vitreous and therefore do not reach the retina. Short-wavelength, high energy visible, blue light (380-500nm) has enough energy per photon (>2.5 eV) to cause damage to cells and tissues known as photochemical damage.
Photochemical damage typically manifests through the creation of reactive oxygen species and free radicals, which can damage proteins, cell membranes, RNA, DNA and mitochondrial DNA. The accumulation of damage to DNA and mitochondrial DNA has been linked to the process of aging (free radical theory of aging) and is thought to play a role in the aetiology of age-related macular degeneration.
.jpg)
Research, showing evidence of photochemical damage, has been performed on molecules, cells and tissues all the way to whole animals including primates and humans. These studies consistently provide evidence that short term high-intensity blue light causes photochemical damage, and that blue light is more dangerous than longer wavelengths. Evidence for long-term low intensity (type I) photochemical damage leading to age-related macular degeneration (AMD) in humans has been obtained from epidemiological studies.
Controlled studies of long-term photochemical damage are not possible in humans due to the length of time required for such studies (>50 years), however, research with monkeys, which has eyes that are structurally identical to our own, has shown that blue light can cause early signs of macular degeneration (lipofuscin and drusen accumulation). In these controlled studies, the maculae were exposed to greater amounts of blue light through a reduction in macular pigments, removed by eliminating carotenoids from the monkeys' diet, compared to control groups that had a normal diet.
These studies have shown that in the absence of blue light protection, early signs of AMD can occur at half the age (human age equivalent of 35 instead of 65 years of age). Humans also have macular pigments that are our natural blue light and antioxidant defence system.
Interested in learning more? Check out some of our related topics
References
- Rozanowska, M., J. Wessels, et al. (1998). "Blue light-induced singlet oxygen generation by retinal lipofuscin in non-polar media." Free Radical Biology and Medicine24(7-8): 1107-1112.
- Boulton, M., M. Rozanowska, et al. (2001). "Retinal photodamage." Journal of Photochemistry and Photobiology B Biology 64(2-3): 144-161.
- Paulus and de Jong 2006 Age-Related Macular Degeneration. New England Journal of Medicine 355:1474-1485
- Algvereet al. 2016 Drusen maculopathy: a risk factor for visual deterioration. Acta Ophthalmol94: 427–433
